GDNF trial - results explained
Between 2012 and 2017, a pioneering clinical trials programme investigated whether delivering an experimental treatment called GDNF directly to the brain could slow, stop or reverse Parkinson’s.
The results are complex but offer hope that it may be possible to restore the cells damaged in Parkinson’s. In this blog, we take a closer look at the results and discuss what might come next.
Short summary if you’re in hurry:
- The GDNF clinical trial tested an experimental new treatment that was infused directly into the brain using pioneering surgery and a purpose-built delivery system.
- Early results after the first 9 months failed to show a significant difference between the GDNF treatment and placebo. However, these initial results only scratched the surface of what was really going on.
- Full analysis of the data shows that GDNF was more successfully delivered than in previous trials and appears to help dopamine-producing cells to regrow.
- Over the course of the trial, the 41 participants experienced substantial improvements in their symptoms and everyday lives.
- The full results highlight that GDNF may yet offer hope to reawaken and restore the brain cells that are gradually destroyed in the condition. To make this a reality, we’re working with partners to push for future trials of GDNF.
A brief history of GDNF
GDNF (or glial cell line-derived neurotrophic factor) is a growth factor, a special protein that is naturally produced inside the brain and supports the survival of many types of brain cells, including the cells lost in Parkinson’s.
Lab studies have suggested that when GDNF is given to brain cells it has the ability to encourage these cells to grow again and may be able to stop the progression of Parkinson’s, something no current treatment can do. But, because GDNF is a large protein, it cannot reach the brain if taken in a pill or injected into a vein. This means it needs to be delivered directly to the brain using a surgical approach.
Previous attempts to get GDNF into the brain to treat Parkinson’s included trials in the early 2000s in which participants had tubes, or catheters, implanted into their brains, enabling GDNF to be slowly but constantly infused from a reservoir pump in their stomach.
However, at the end of these trials, the GDNF treatment did not show benefit over placebo treatment. One reason for this may have been the slow rate of the infusions, which allowed the GDNF to reach cells within only a few millimetres of the catheter tip. This would have meant the majority of the target brain area — a walnut-sized region called the putamen — would have been left untreated.

To address this challenge, neurosurgeon Professor Steven Gill, designed a sophisticated new delivery system. Instead of a slow but constant flow of GDNF, the new delivery system used a process called Convection Enhanced Delivery (CED) to allow a full month’s dose of drug to be delivered in around 2 hours. The idea being that delivering GDNF at higher pressure would help it penetrate the brain tissue better.
Armed with this new purpose-built delivery system, at last, new clinical trials were ready to commence. The new studies were led by Dr Alan Whone and his team at North Bristol NHS Trust, and split into 3 distinct stages:
Safety pilot
6 participants were involved in an initial safety and feasibility study to ensure that the surgery, device and drug were safe and acceptable to patients, and also to check that the drug delivery system was working as intended.
Main study
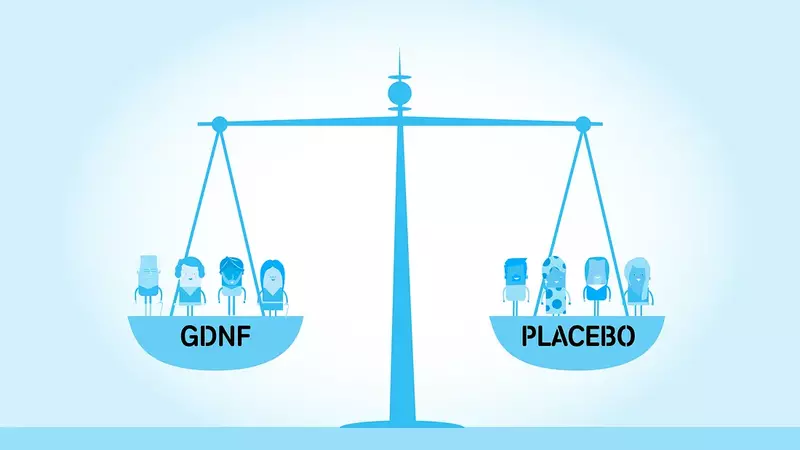
Next 35 participants were recruited to the main study: a 9-month double-blind placebo-controlled trial. The 35 participants were randomly assigned by computer to receive monthly infusions over the course of 9 months of either the active drug (GDNF) or a placebo (an artificial form of the cerebrospinal fluid that surrounds the brain). Crucially, during this phase, neither the medical team nor the participants knew which they were receiving.
Open label extension
Once participants had completed the 9-month double-blind study, they were offered the opportunity to continue into an extension study in which all participants received GDNF for a further 9 months. During this part of the trials, both the participants themselves and the researchers knew that everyone would be receiving GDNF and this is why it’s called ‘open label’.
The results
The study was successfully completed in February 2017 and the full findings were published in February 2019 in leading scientific journals Brain and Journal of Parkinson’s Disease.
- Read the full open access paper in Brain, on the Oxford Academic website.
- Read the full open access paper in Journal of Parkinson’s Disease on the IOS Press website.
GDNF not significantly better than placebo
Early results from the first 9-month double-blind phase of the trial, published in July 2017, were ultimately disappointing. Initial analysis suggested that the treatment is safe but while those who received GDNF improved more than the placebo group over the 9 months, the difference between the 2 groups was not large enough to be statistically significant.
‘Statistical significance’ is a mathematical test that helps us decide whether a result is real or could be due to chance. For any new treatment to prove its worth, it must be shown to be better than a placebo by a sufficient margin to achieve statistical significance.
In this trial, to achieve statistical significance, the GDNF group needed to have improved by 20% more than the placebo group in their movement score when assessed off their regular Parkinson’s medication after 9 months. The results actually showed the GDNF group improved about 5% more than the placebo group so it was quite a long way from achieving statistical significance.
However, the initial results only scratched the surface of the huge amount of information collected throughout the study, which has generated over 20,000 sheets of data. And, despite the disappointment of this central result, when you look a little deeper there are some compelling signs that GDNF may have exciting beneficial effects.
Brain scans reveal positive effects on damaged brain cells
All participants had specialised brain scans (called PET) before starting the trial and after 9 months. Participants had an injection of a radioactive version of dopamine (18F-dopa) so that the PET scanner could then track the movement of dopamine through their brains.
After 9 months, there was no change in the scans of those who received placebo, whereas the group who received GDNF showed an improvement of 100% in the targeted part of the putamen, and between 20 and 50% improvement in the rest of this brain area. Crucially, these improvements were statistically significant.
This finding shows that the device successfully delivered the drug to the target brain area and that GDNF was having a biological effect on cells.
The improvement in the brain scans may indicate that GDNF may be helping damaged cells to grow new connections, restore hibernating connections, produce more dopamine, or a combination of all 3.
This offers real hope that it may be possible to reawaken and restore damaged brain cells in Parkinson’s but to prove that GDNF is an effective treatment these improvements in brain scans need to be reflected in measurable benefits for those living with the condition.
Positive trends in favour of GDNF across almost all assessments
Those who received GDNF showed greater improvements than the placebo group in almost all clinical assessments throughout the 9-month double-blind period.
These assessments included measures of:
- movement symptoms such as tremor, walking, slowness, stiffness and dexterity
- non-movement aspects of the condition such as mood, thinking, memory, pain and sleep
- ability to perform everyday activities and quality of life using questionnaires completed by participants
- how well regular medication was working, measured using participant diaries.
Although, the difference between the 2 groups was not big enough to be conclusive (statistically significant) on any of these individual assessments. The fact that the GDNF group seemed to be doing better than the placebo group across the board is encouraging.
Substantial improvements in symptoms at 18 months
After the initial 9 months on either GDNF or placebo, all 41 participants chose to continue into the second ‘open label’ phase of the study in which all received a further 9 months on GDNF.
During this period, participants continued to undergo assessments of their Parkinson’s every 8 weeks.
By the end of this second 9-month period, both groups showed moderate to large improvements in symptoms and ability to perform everyday activities compared to their scores at the start of the studies.
The scale of these improvements is encouraging but because participants knew they were receiving GDNF in the second 9 months they need to be treated with caution as they could be due to the placebo effect.
A device that can deliver drugs to the brain with pinpoint precision
The trial involved pioneering, robot-assisted brain surgery to fit a specially-designed delivery device to deliver the drug with pinpoint accuracy to the particular part of the brain affected in Parkinson’s. Participants had 4 tubes carefully placed into their brains that are connected to a small port behind their ear, allowing GDNF to be pumped directly through the tubes to the affected brain areas with pinpoint accuracy.
The trials have shown that this delivery method is very effective for consistently delivering GDNF at the right concentration to the right part of the brain, even after 9 months of treatment.
This delivery method has the potential to treat a wide range of other brain conditions. It has already been used to treat some adults and children with otherwise inoperable brain cancer and is now being used to deliver another growth factor therapy (called CDNF) for Parkinson’s in a clinical trial underway in Scandinavia.
GDNF treatment appears to be safe and acceptable
Finally, despite the incredible commitment involved in taking part in this complex and intensive study, all the participants enrolled in the study completed it.
Over the course of the trial, the clinical team administered more than 1,000 infusions in total. Participants visited the trial centre for these infusions once every 4 weeks for 18 months and remarkably 99% of GDNF infusions were successfully administered and there were no serious side effects from the study drug.
What happens next?
These results are not clear-cut but they hold real promise for people with Parkinson’s that deserves further exploration.
The major improvements seen in the brain scans, coupled with the benefits in symptoms after 18 months, offer hope that it may be possible to reawaken and restore the brain cells that are gradually destroyed in the condition.
To move this experimental therapy forward, we now need further trials to provide conclusive evidence of the benefits of GDNF.
Considerations for future trials
For GDNF to move forward as quickly as possible we need to make sure that future studies address the questions raised by these results and deliver definitive results. This means working with the international research community and with people affected by Parkinson’s to reflect and learn from these results and to get the plan for further studies absolutely right. And there are a number of things to consider when planning future studies.
Tackling the placebo effect
The ‘placebo effect’ is a major challenge in all clinical trials. The expectation of receiving a new and potentially beneficial treatment actually triggers a physiological response that can make us better.
In the recent GDNF trial, the placebo response was significant. On average the placebo group participants' movement symptoms had improved by around 12% after 9 months when they were measured when off their regular Parkinson’s drugs.
Previous studies have shown that the placebo response can be particularly profound in people with Parkinson’s, and also that it can be exacerbated if the treatment is expensive, invasive or involves lots of contact with professionals, all of which apply in this case and may have strengthened the response in this trial.
The right participants
Another key consideration for all trials, and especially in Parkinson’s, is ensuring you select the right people to take part in your trial.
In the recent trials, there was quite a wide variation in the response in both groups, with some individuals experiencing profound improvements and others not. Although the researchers did further analysis to investigate whether there were any possible explanations for this, for example, whether younger people or participants at an earlier stage of their Parkinson’s did better, they did not find any clear patterns.
The right assessments
The research team used internationally recognised assessment tools and aimed to capture as much information as possible about the impact of GDNF in these trials.
But, as we’ve blogged about previously, there is a lot of room for improvement in terms of how Parkinson’s symptoms and the impact of the condition on daily life is captured in clinical trials.
Better measurement tools are urgently needed for Parkinson’s to help us capture the full impact of treatments like GDNF, and that means developing them in partnership with patients and their families. There are already a number of projects happening across the world that aim to do this using various approaches, including the use of digital technology to monitor the condition and creating brand new patient-reported outcome measures, so there is a growing range of better tools on the horizon.
Dose, length, size
Finally, as with any clinical trial, one of the fundamental (and trickiest) aspects is deciding:
- how many participants you need
- what dose (or doses) of your treatment to test
- how long to run your trial.
In the recent trial, the results indicate that the device successfully delivered the drug to the right brain cells and produced positive biological effects as seen in the brain scans.
But although there were improvements in symptoms, the results did not show the same clear-cut difference between the GDNF and placebo groups at 9 months.
One possible explanation for this is that if GDNF was indeed helping to revive and restore damaged brain cells, perhaps improvements in symptoms may lag behind biological effects.
Perhaps a larger study, a higher dose of GDNF, or a longer ‘double-blind’ period would provide a better chance of seeing a clear difference between the groups, and these are all factors that need to be carefully considered in planning future studies.
Support our vital research
We’re proud pioneers behind the GDNF trial and we’ll leave no stone unturned in our search for a cure. But we can’t do it without you. Make life-changing breakthroughs happen.

